Chronic Obstructive Pulmonary Disease (COPD): Causes, Symptoms & Treatment Guide 2026

Chronic Obstructive Pulmonary Disease (COPD)
is a long-term, progressive lung condition which makes breathing difficult over the due course of time. Currently spreading worldwide, with significant unawareness leading to impact daily life of human being. COPD is affected primarily for adults above the age of 40, in close contact with long term exposure to lung irritants such as tobacco smoke, air pollution, and occupational chemicals.
This comprehensive blog explains what COPD is, why it develops, how it is diagnosed, and all treatment options available today, including a complete list of COPD medications with American brand names and compositions, presented in a medically accurate and regulatory-safe manner.
What Is COPD?
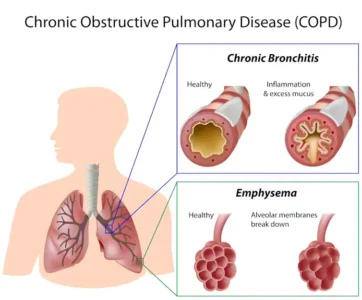
COPD is a collective term used to describe chronic lung diseases that cause persistent airflow limitation. The two most common conditions under COPD are:
- Chronic Bronchitis – long-term inflammation of the airways with excessive mucus production
- Emphysema – destruction of the air sacs (alveoli) in the lungs, reducing oxygen exchange
Most people with COPD have a combination of both conditions. The disease is rapidly progressive, meaning symptoms typically worsen over time, but early diagnosis and appropriate management can significantly slow progression and improve quality of life.
What are the Causes of Chronic Obstructive Pulmonary Disease (COPD)
COPD develops with long term usage/exposure to substances responsible for irritation and lung damage. Unlike sudden respiratory illnesses, COPD is the result of long-term accumulated lung injury for over the years, which resemble with the symptoms appearance often later in life. Understanding the causes is essential not only for prevention but also for slowing disease progression after diagnosis.
- Tobacco Smoking (Most Common Primary Cause)
Cigarette smoking is the single largest risk factor for COPD worldwide. Long-term inhalation of tobacco smoke causes:
- Chronic inflammation of the airways
- Damage to the alveoli (air sacs)
- Excess mucus production
- Narrowing and scarring of bronchial tubes
Cigarette smoking, or use of tobacco related products which contains harmful chemicals that attacks and weakens the lung’s natural defence mechanism. With overtime usage, it causes irreversible blockage in airflow. Irrespective of situation, current and former smokers are always in risk with COPD, although quitting smoking early can slow down disease progression. There are several medications available to reduce smoking cessation like Naltrexone Tablets, LDN tablets, Bupropion (Zyban) and Varenicline (Champix)
Passive exposure or someone smoking in your surrounding for over a period of time which causes an indirect inhalation of toxic fumes and also contributes to COPD, particularly in people exposed from childhood.
- Long-Term Exposure to Air Pollution
Environmental air pollution is an increasingly recognized contributor to COPD, especially in urban and industrial regions where the air contains harmful fumes and chemicals omitted by several sources. Common sources include:
- Vehicle emissions
- Industrial smoke and chemicals
- Burning of biomass fuels (wood, coal, dung)
Indoor air pollution is a major risk factor in low- and middle-income countries, where poorly ventilated homes expose individuals—especially women and children—to harmful smoke daily for years.
- Occupational Dust, Fumes, and Chemicals
COPD at professional workplace which involves usage of materials/goods which acts as irritants repeatedly leading to higher risk of COPD. Common in professions like :
- Construction and mining
- Agriculture and farming
- Textile and chemical manufacturing
- Welding, metalworking, and painting industries
Insufficient safety equipment’s, and prolonged working hours can cause the lung damage even in the case of non-smoker.
- Genetic Factors (Alpha-1 Antitrypsin Deficiency)
A small percentage of COPD cases are linked to alpha-1 antitrypsin deficiency, a genetic condition that reduces the lungs’ ability to protect themselves from inflammation-related damage. People with this condition may develop COPD at a younger age, sometimes without any history of smoking.
- Early-Life Lung Infections and Poor Lung Development
Respiratory infections during childhood, premature birth, or exposure to pollutants during early lung development can result in reduced lung capacity later in life. These individuals may develop COPD symptoms earlier or experience more severe disease degree progression.

Symptoms of Chronic Obstructive Pulmonary Disease (COPD): Early to Advanced Stages
COPD symptoms vary widely between individuals and often worsen over the duration of time. Many people adapt unknowingly, limiting activity to avoid discomfort—leading to delayed diagnosis.
Early-Stage Symptoms
In the early stages, symptoms may be mild and intermittent:
- Feeling shortness of breath with physical activity quicky
- Smoker’s cough / Chronic cough development
- Mild chest tightness
- Over production of mucus, especially in the morning
Because these symptoms develop slowly, many people do not seek medical care until lung damage is already significant.
Moderate Symptoms
As Chronic Obstructive Pulmonary Disease (COPD) progresses, symptoms become more noticeable and frequent:
- Shortness of breath during routine activities (walking, climbing stairs)
- Persistent cough with thick mucus
- Wheezing or whistling sounds during breathing
- Frequent respiratory infections (bronchitis, pneumonia)
- Fatigue due to reduced oxygen delivery
At this stage, COPD begins to interfere with daily life and work productivity.
Advanced and Severe Symptoms
In later stages, COPD can cause severe functional limitations:
- Increased breathing even at rest
- Difficulty speaking full sentences
- Bluish lips or fingernails (low oxygen levels)
- Swelling in ankles and feet
- Unintended weight loss and muscle weakness
- Anxiety, depression, and sleep disturbances
Acute flare-ups, known as COPD exacerbations, may occur—often triggered by infections or air pollution—and may require hospitalization.
Prevention Strategies for Chronic Obstructive Pulmonary Disease (COPD)
Although COPD-related lung damage cannot be reversed, prevention remains the most powerful tool in reducing disease burden. Many cases of COPD are preventable through lifestyle and environmental interventions.
- Avoid Tobacco Exposure Completely
- Never start smoking
- Quit smoking as early as possible if currently smoking
- Avoid secondhand smoke at home, work, and public places
Smoking cessation is the most effective intervention to prevent COPD and slow progression in diagnosed individuals.
- Improve Indoor Air Quality
- Use clean cooking fuels and proper ventilation
- Avoid burning wood, coal, or biomass indoors
- Use exhaust fans or chimneys where applicable
Improving household air quality significantly reduces long-term lung damage, especially in developing regions.
- Minimize Occupational Exposure
- Use protective masks and ventilation systems
- Follow workplace safety guidelines
- Undergo regular health screenings if working in high-risk environments
Employers and employees share responsibility for reducing inhalation exposure.
- Reduce Outdoor Pollution Exposure
- Limit outdoor activity during high-pollution days
- Use air purifiers indoors when possible
- Support clean-air initiatives and environmental regulations
Climate change and air pollution are increasingly linked to respiratory disease severity.
- Vaccinations and Infection Prevention
Respiratory infections can accelerate lung damage and trigger COPD exacerbations.
Recommended preventive measures include:
- Annual influenza vaccination
- Pneumococcal vaccination as advised
- Prompt treatment of respiratory infections
- Early Screening for At-Risk Individuals
People with long-term smoking history or occupational exposure should undergo lung function testing, even if symptoms are mild. Early detection enables earlier intervention and better long-term outcomes.
Why Early Prevention and Awareness Matters in Chronic Obstructive Pulmonary Disease (COPD)
COPD is often underdiagnosed until advanced stages, when lung damage is extensive. Public awareness, early screening, and risk reduction strategies can:
- Delay disease onset
- Reduce healthcare burden
- Improve long-term survival
- Enhance quality of life
Prevention-focused education plays a critical role in combating the global rise of Chronic Obstructive Pulmonary Disease (COPD).
Complete List of COPD Medications (With U.S. Brand Names & Compositions)

COPD medications fall into several well-defined categories. These medications are prescribed by healthcare professionals and are used either as rescue therapy or long-term maintenance treatment.
- Short-Acting Bronchodilators (Rescue Medications)
Used for quick relief of sudden breathing difficulty.
Short-Acting Beta-Agonists (SABA):
- ProAir HFA – Albuterol sulfate
- Ventolin HFA – Albuterol sulfate
- Xopenex HFA – Levalbuterol tartrate
Short-Acting Anticholinergics (SAMA):
- Atrovent HFA – Ipratropium bromide
Combination Rescue Inhaler:
- Combivent Respimat – Albuterol + Ipratropium
- Long-Acting Bronchodilators (Maintenance Therapy)
Used daily to keep airways open over time.
Long-Acting Beta-Agonists (LABA):
- Serevent Diskus – Salmeterol xinafoate
- Foradil Aerolizer – Formoterol fumarate
- Arcapta Neohaler – Indacaterol maleate
- Striverdi Respimat – Olodaterol
Long-Acting Muscarinic Antagonists (LAMA):
- Spiriva HandiHaler / Respimat – Tiotropium bromide
- Incruse Ellipta – Umeclidinium bromide
- Tudorza Pressair – Aclidinium bromide
- Seebri Neohaler – Glycopyrrolate
- LABA + LAMA Combination Inhalers
Commonly prescribed for moderate to severe COPD.
- Anoro Ellipta – Umeclidinium + Vilanterol
- Stiolto Respimat – Tiotropium + Olodaterol
- Bevespi Aerosphere – Glycopyrrolate + Formoterol
- Duaklir Pressair – Aclidinium + Formoterol
- Inhaled Corticosteroids (ICS)
Used in selected patients with frequent exacerbations (not as monotherapy).
- Flovent HFA – Fluticasone propionate
- Pulmicort Flexhaler – Budesonide
- QVAR RediHaler – Beclomethasone dipropionate
- LABA + ICS Combination Inhalers
- Advair Diskus / HFA – Fluticasone + Salmeterol
- Symbicort – Budesonide + Formoterol
- Breo Ellipta – Fluticasone furoate + Vilanterol
- Dulera – Mometasone + Formoterol
- Triple Therapy Inhalers (LABA + LAMA + ICS)
Used in severe COPD or frequent flare-ups.
- Trelegy Ellipta – Fluticasone furoate + Umeclidinium + Vilanterol
- Breztri Aerosphere – Budesonide + Glycopyrrolate + Formoterol
- Oral Medications
- Daliresp – Roflumilast (PDE-4 inhibitor to reduce inflammation)
- Theo-24 – Theophylline (limited use due to safety considerations)
- Supportive Medications
- Mucolytics: Acetylcysteine
- Expectorants: Guaifenesin
- Antibiotics (during bacterial exacerbations only):
Azithromycin, Amoxicillin-Clavulanate, Levofloxacin
Lifestyle Management and Long-Term Care
Effective COPD management also includes:
- Smoking cessation
- Pulmonary rehabilitation
- Vaccinations (influenza, pneumococcal)
- Regular physical activity
- Oxygen therapy for advanced disease
- Mental health and emotional support
Prevention and Risk Reduction
- Avoid tobacco smoke and pollutants
- Use protective equipment at workplaces
- Seek early medical evaluation for chronic cough or breathlessness
- Maintain regular follow-ups if at risk
Final Thoughts
COPD is a serious but manageable condition. With early diagnosis, evidence-based medications, and lifestyle adjustments, many people with COPD continue to lead active and fulfilling lives. Ongoing collaboration with healthcare professionals is essential for long-term disease control.

.svg)